Personal Health Care – Spending > on Key Conditions
 Personal Health Care
Personal Health Care
Spending on Personal Health Care, Public Health Increases Substantially
Estimates of U.S. spending on individual health care and public health showed substantial increases from 1996 through 2013, with spending on diabetes, ischemic heart disease, and low back and neck pain accounting for the highest amounts of spending by disease category, according to a study appearing in the December 27 issue of JAMA.
Health care spending in the United States is greater than in any other country in the world. According to estimates, spending on health care accounted for more than 17 percent of the U.S. economy in 2014. Between 2013 and 2014 alone, spending on health care increased 5.3 percent. Despite the resources spent on health care, much remains unknown about how much is spent for each condition, or how spending on these conditions differs across ages and time. Understanding how health care spending varies can help health system researchers and policy makers identify which conditions, age and sex groups, and types of care are driving spending increases.
Joseph L. Dieleman, Ph.D., of the Institute for Health Metrics and Evaluation, University of Washington, Seattle, and colleagues estimated U.S. spending on personal health care and public health, according to condition (i.e., disease or health category), age and sex group, and type of care. Government budgets, insurance claims, facility surveys, household surveys, and official U.S. records from 1996 through 2013 were collected and combined. In total, 183 sources of data were used to estimate spending for 155 conditions (including cancer, which was disaggregated [to divide into parts] into 29 conditions).
From 1996 through 2013, $30.1 trillion of personal health care spending was disaggregated by 155 conditions, age and sex group, and type of care. Among these conditions, diabetes had the highest health care spending in 2013, with an estimated $101.4 billion in spending, including 57.6 percent spent on pharmaceuticals and 23.5 percent spent on ambulatory care. Ischemic heart disease accounted for the second-highest amount of health care spending in 2013, with estimated spending of $88.l billion, and low back and neck pain accounted for the third-highest amount, with estimated health care spending of $87.6 billion.
The conditions with the highest spending levels varied by age, sex, type of care, and year. Personal health care spending increased for 143 of the 155 conditions from 1996 through 2013. Spending on low back and neck pain and on diabetes increased the most over the 18 years, by an estimated $57.2 billion and $64.4 billion, respectively. From 1996 through 2013, spending on emergency care and retail pharmaceuticals increased at the fastest rates (6.4 percent and 5.6 percent annual growth rate, respectively), which were higher than annual rates for spending on inpatient care (2.8 percent) and nursing facility care (2.5 percent).
The treatment of 2 risk factors, hypertension and hyperlipidemia, were also among the top 20 conditions incurring spending. Spending for these conditions has collectively increased at more than double the rate of total health spending, and together led to an estimated $135.7 billion in spending in 2013.
“The rate of change in annual spending varied considerably among different conditions and types of care. This information may have implications for efforts to control U.S. health care spending,” the authors write.
Cataract Symptoms – Depression is a Side Effect
 Cataract Symptoms Depression
Cataract Symptoms Depression
Cataract Symptoms have a side impact – older adults who are more likely to have symptoms of depression, reports a study in Optometry and Vision Science, the official journal of the American Academy of Optometry.
The link between cataracts and depression is independent of other factors, and appears strongest among older adults with lower education, according to new research by Haifang Wang, MSc, of Soochow University, Suzhou, China, and colleagues. They write, “[O]ur study sheds further light on the complex relationship between aging, vision loss, cataract, and depression and suggests that there may be a role for cataract surgery in improving mental health in the elderly.”
Increased Depressive Cataract Symptoms in Older Adults with Cataracts
Age-related cataracts are the leading cause of visual impairment worldwide and are expected to increase as population demographics shift towards advancing age. Depression is also common in older adults. This large study in Chinese older adults investigated the link between visual impairment and cataract symptoms of depression and provides evidence for an association between cataracts and depression.
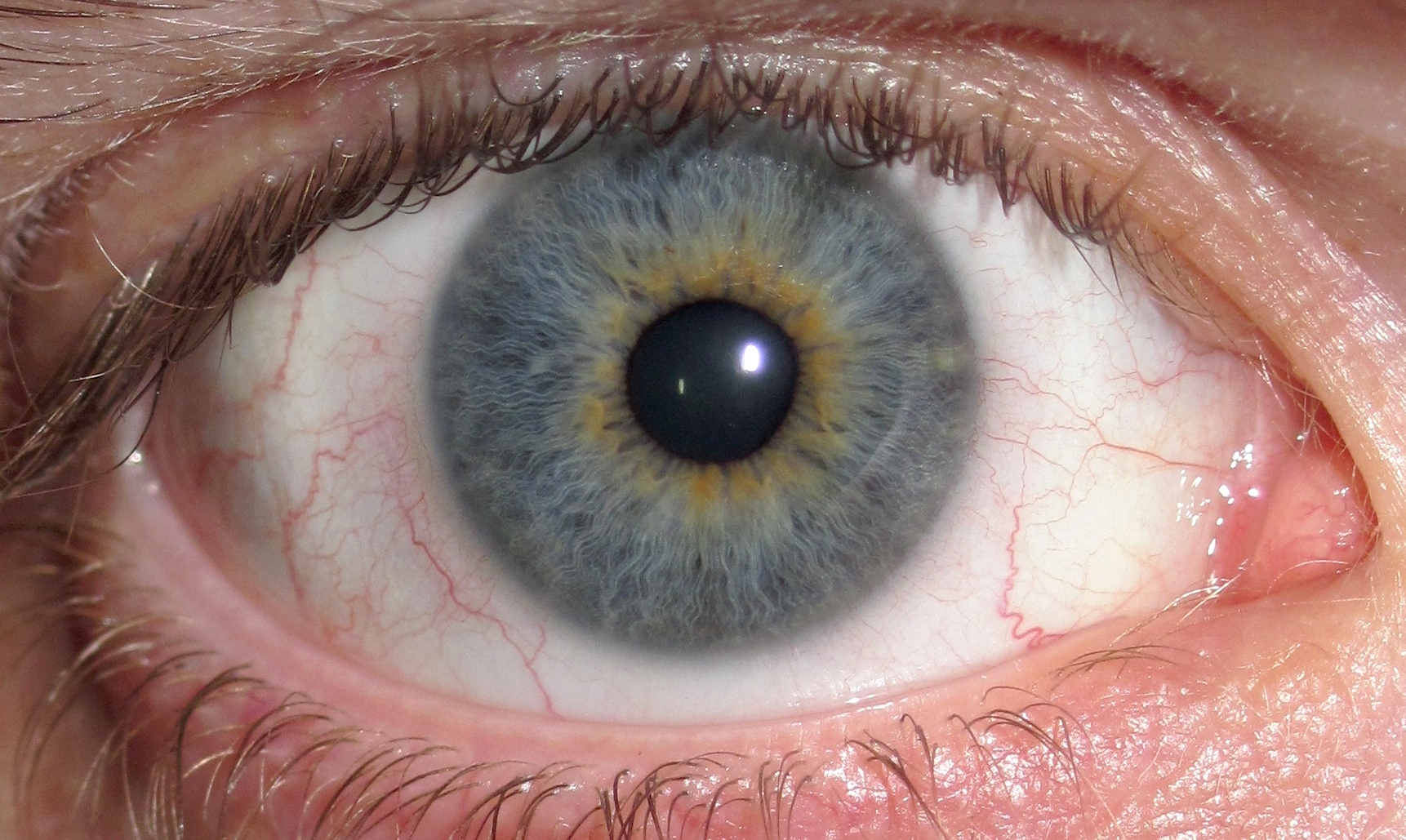
As part of a community survey study, approximately 4,600 older adults (60 years or older) in one Chinese town completed a depression questionnaire. Participants also underwent a clinical eye examination to rate the presence and severity of cataracts. Cataracts are a very common condition in older adults, with clouding of the lens of the eye causing vision loss.
Excluding those with previous cataract surgery, nearly half (49 percent) of older adults in the study had cataracts in at least one eye. On the depression questionnaire, 8 percent of subjects had depressive symptoms. Symptoms of depression were more common in women than men and more common in older age groups.
Older adults with cataracts were more likely to have depressive symptoms, independent of socioeconomic status, lifestyle factors, and visual acuity. On adjusted analysis, symptoms of depression were 33 percent more likely when cataracts were present. Importantly, the odds of depressive symptoms were similar for subjects with cataracts in one eye versus both eyes.
The association between cataracts and depression was even stronger for subjects with no formal education–a 50 percent increase. After all other factors were taken into account, cataracts explained 14 percent of the variation in depression risk.
The researchers note that their study cannot show the direction of the association–vision loss might cause older adults to become isolated and withdrawn, or depression might make them less likely to seek treatment for cataracts.
“These results suggest that optometrists and vision care professionals should think beyond the direct effects of cataracts on visual impairment. We should also consider the broader impact that vision loss may have on mental health and well-being,” comments Michael Twa, OD, PhD, FAAO, Editor-in-Chief of Optometry and Vision Science. “As a next step, it would be important to know if the associated depression in older adults is reversible following the restoration of vision after cataract surgery.”
Fall Prevention – Brain Activity May Predict Risk of Falls
Fall Prevention – Brain Activity May Predict Risk of Falls in Older People
When it comes to fall prevention, measuring the brain activity of healthy, older adults while they walk and talk at the same time may help predict their risk of falls later, according to a study published in the online issue of Neurology®, the medical journal of the American Academy of Neurology.
“In older people who had no signs of disease that would make them prone to falls, higher levels of activity in the front of the brain, called the prefrontal cortex, were associated with a higher risk of falls later in life,” said study author Joe Verghese, MBBS, MS of the Albert Einstein College of Medicine in the Bronx, NY, and Fellow of the American Academy of Neurology. “This suggests that these people were increasing their activation of brain cells or using different parts of the brain to compensate for subtle changes in brain functioning.”
The prefrontal cortex is the area of the brain where goal setting and decision-making takes place.
For the study, researchers looked at 166 people with an average age of 75 who had no disabilities, dementia or problems with walking.
Over that time, 71 people in the study reported 116 falls; 34 people fell more than once. Most falls were mild with only 5 percent resulting in fractures.
The study found higher levels of brain activity while both walking and talking were associated with falls, with each incremental increase of brain activity associated with a 32 percent increased risk of falls. Such an association was not found when looking at brain activity levels during just walking or talking.
The relationship between brain activity and falls risk was the same after researchers accounted for other factors that could affect a person’s risk of falling, such as slow walking speed, frailty and previous falls.
“These findings suggest that there may be changes in brain activity before physical symptoms like unusual gait appear in people who are more prone to falls later,” said Verghese.
I am not sure exactly what to make of this. Sort of like “I can walk and chew gum too!” Maybe this study is suggesting we can’t. The more multi-tasking we do, the more distracted we are, the more prone to falls we become. That’s my take.
Our Friday Song of the Week – Go Your Own Way
Go Your Own Way – Fleetwood Mac
Improve Memory – Exercise May Help Ward Off Memory Decline
Improve Memory
Exercise may be associated with a small benefit for elderly people who already have memory and thinking problems, according to new research in Neurology®, a medical journal of the American Academy of Neurology. The research involved people with vascular cognitive impairment, which is the second most common cause of dementia after Alzheimer’s disease.
All of the participants were tested before the study started, at the end of the study and again six months later on their overall thinking skills, executive function skills such as planning and organizing and how well they could complete their daily activities.
Those who exercised did improve memory slightly on the test of overall thinking skills compared to those who did not exercise.









