Joy Filled Dementia Visits – Smilecast 143
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Our Friday Song of the Week – A Thousand Years
Our Friday Song of the Week – A Thousand Years
Exercise and Thinking Skills – How Much is Enough?
 How Much Exercise Is Needed to Help Improve Thinking Skills?
How Much Exercise Is Needed to Help Improve Thinking Skills?
We know that exercise may help improve thinking skills. But how much exercise? And for how long? To find the answers, researchers reviewed all of the studies where older adults were asked to exercise for at least four weeks and their tests of thinking and memory skills were compared to those of people who did not start a new exercise routine. The review is published in the online issue of Neurology® Clinical Practice.
They found that people who exercised an average of at least 52 hours over about six months for about an hour each session may improve their thinking skills.
In contrast, people who exercised for an average of 34 hours over the same time period did not show any improvement in their thinking skills.
The review did not find a relationship between a weekly amount of exercise and improved thinking skills.
“These results suggest that a longer-term exercise program may be necessary to gain the benefits in thinking skills,” said study author Joyce Gomes-Osman, PT, PhD, of the University of Miami Miller School of Medicine in Florida. “We were excited to see that even people who participated in lower intensity exercise programs showed a benefit to their thinking skills. Not everyone has the endurance or motivation to start a moderately intense exercise program, but everyone can benefit even from a less intense plan.”
The review included 98 randomized, controlled trials with a total of 11,061 participants with an average age of 73. Of the total participants, 59 percent were categorized as healthy adults, 26 percent had mild cognitive impairment and 15 percent had dementia. A total of 58 percent did not regularly exercise before being enrolled in a study.
Researchers collected data on exercise session length, intensity, weekly frequency and amount of exercise over time. Aerobic exercise was the most common type of exercise, with walking the most common aerobic exercise and others including biking and dancing. Some studies used a combination of aerobic exercise along with strength, or resistance training and some used strength training alone. A small number of studies used mind-body exercises such as yoga or Tai chi.
After evaluating all of the data, researchers found that in both healthy people and people with cognitive impairment longer term exposure to exercise, at least 52 hours of exercise conducted over an average of about six months, improved the brain’s processing speed, the amount of time it takes to complete a mental task. In healthy people, that same amount of exercise also improved executive function, a person’s ability to manage time, pay attention and achieve goals. However, researchers found no link between the amount of exercise and improved memory skills. Aerobic exercise, strength training, mind-body exercise and combinations of these were all found to be beneficial to thinking skills.
“Only the total length of time exercising could be linked to improved thinking skills,” said Gomes-Osman. “But our results may also provide further insight. With a majority of participants being sedentary when they first enrolled in a study, our research suggests that using exercise to combat sedentary behavior may be a reason why thinking skills improved.”
Shrinkage – of the Brain! Possibly Preventable with the Right Diet
 For Older Adults, a Better Diet May Prevent Brain Shrinkage
For Older Adults, a Better Diet May Prevent Brain Shrinkage
People who eat a diet rich in vegetables, fruit, nuts and fish may have bigger brains, according to a study published in Neurology®.
“People with greater brain volume have been shown in other studies to have better cognitive abilities, so initiatives that help improve diet quality may be a good strategy to maintain thinking skills in older adults,” said study author Meike W. Vernooij, MD, PhD, of the Erasmus University Medical Center in Rotterdam, the Netherlands. “More research is needed to confirm these results and to examine the pathways through which diet can affect the brain.”
The study included 4,213 people in the Netherlands with an average age of 66 who did not have dementia.
Participants completed a questionnaire asking how much they ate of nearly 400 items over the past month. Researchers looked at diet quality based on the Dutch dietary guidelines by examining intake of foods in the following groups: vegetables, fruit, whole grain products, legumes, nuts, dairy, fish, tea, unsaturated fats and oils of total fats, red and processed meat, sugary beverages, alcohol and salt. Researchers ranked the quality of diet for each person with a score of zero to 14. The best diet consisted of vegetables, fruit, nuts, whole grains, dairy and fish, but a limited intake of sugary drinks. The average score of participants was seven.
All participants had brain scans with magnetic resonance imaging to determine brain volume, the number of brain white matter lesions and small brain bleeds. The participants had an average total brain volume of 932 milliliters.
Information was also gathered on other factors that could affect brain volumes, such as high blood pressure, smoking and physical activity.
Researchers found after adjusting for age, sex, education, smoking and physical activity that a higher diet score was linked to larger total brain volume, when taking into account head size differences. Those who consumed a better diet had an average of two milliliters more total brain volume than those who did not. To compare, having a brain volume that is 3.6 milliliters smaller is equivalent to one year of aging.
For comparison, researchers also assessed diet based on the Mediterranean diet, which is also rich in vegetables, fish and nuts, and found brain volume results were similar to those who adhered closely to Dutch dietary guidelines.
Vernooij said the link between better overall diet quality and larger total brain volume was not driven by one specific food group, but rather several food groups.
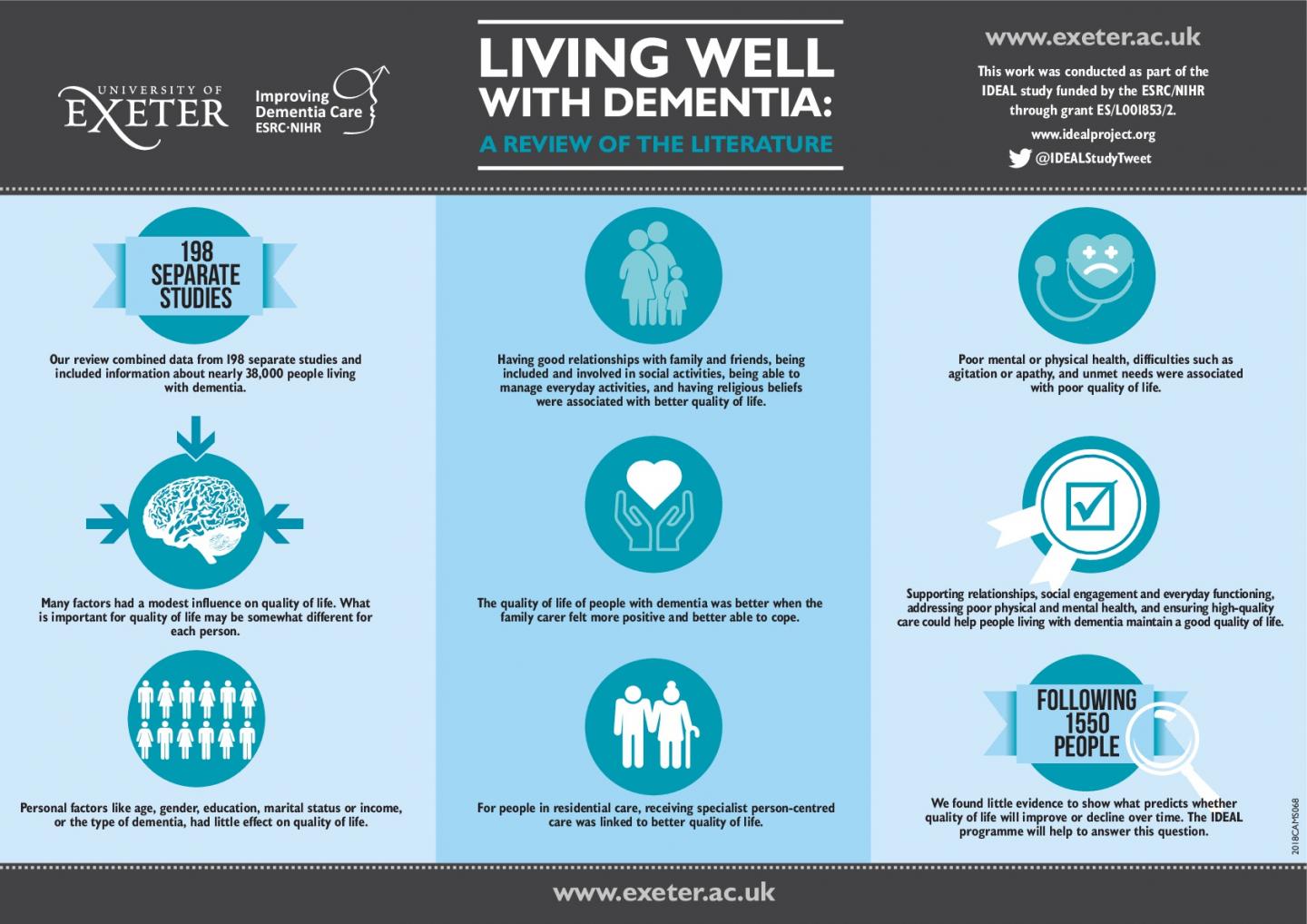
Key Factors to Support Quality of Life in Dementia
Research reveals key factors to support quality of life in dementia
A robust research analysis has identified what factors can be targeted to support people to live as well as possible with dementia.
The study, led by the University of Exeter and published in the journal Psychological Medicine, found that good relationships, social engagement, better everyday functioning, good physical and mental health, and high-quality care were all linked to better quality of life for people with dementia.These are things I speak about in my motivational speech – The Meaning of Life!
Professor Linda Clare, at the University of Exeter, said: “This research supports the identification of national priorities for supporting people to live as well as possible with dementia. While many investigations focus on prevention and better treatments, it’s equally vital that we understand how we can optimise quality of life for the 50 million people worldwide who have dementia. We now need to develop ways to put these findings into action to make a difference to people’s lives by supporting relationships, social engagement and everyday functioning, addressing poor physical and mental health, and ensuring high-quality care.”
The research was supported jointly by the Economic and Social Research Council (ESRC) and the National for Health Research (NIHR). It involved collaboration with the London School of Economics, the universities of Sussex, Bangor, Cardiff, Brunel and New South Wales in Australia, and Kings College London.
The team carried out a systematic review and meta-analysis to examine all available evidence about the factors that are associated with quality of life for people with dementia. They included 198 studies, which incorporated data from more than 37,000 people.
The study found that demographic factors such as gender, education marital status, income or age were not associated with quality of life in people with dementia. Neither was the type of dementia.
Factors that are linked with poor quality of life include poor mental or physical health, difficulties such as agitation or apathy, and unmet needs.
Factors that are linked with better QoL include having good relationships with family and friends, being included and involved in social activities,
being able to manage everyday activities, and having religious beliefs.
Many other factors showed small but statistically significant associations with quality of life. This suggests that the way in which people evaluate their quality of life is related to many aspects of their lives, each of which have a modest influence. It is likely that to some extent the aspects that are most important may be different for each person.
Evidence from longitudinal studies about what predicts whether or not someone will experience a good quality of life at later stages was limited. The best indicator was the person’s initial rating of quality of life. This again highlights the importance of optimising quality of life from the earliest stages of living with dementia.
Dr Anthony Martyr, lead author on the study, from the University of Exeter, said: “While in general it is more of a challenge to maintain good quality of life as dementia progresses, we found little evidence to show what predicts whether quality of life will improve or decline over time. The IDEAL programme we are currently leading will follow people living with dementia over several years and will help to answer this question.”
Dr Doug Brown, Chief Policy and Research Officer at Alzheimer’s Society, said: “Maintaining a healthy social life and doing things you enjoy is important for everyone’s quality of life. As this Alzheimer’s Society funded study highlights, people living with dementia are no exception.
“Someone develops dementia every three minutes but too many are facing it alone and feel socially isolated- a factor that researchers pinpoint contributing to a lower quality of life.
“People with dementia have a right to continue living a life they love. Alzheimer’s Society’s Dementia Friendly Communities initiative enables individuals, businesses and communities to involve and empower people affected – but we need all of society to unite to ensure people with dementia feel understood, valued and able to contribute to their community.”